Treatment vs. Weight Loss Maintenance – What’s the Difference?
I had the pleasure of hearing Dr. Michael Rosenbaum from Columbia University speak at our Obesity Medicine Association Conference on the topic of why maintaining weight loss is so hard. He has been engaged in research on this topic for decades, studying the effects of weight change on body metabolism.
In his studies, after a person has lost weight (and is now in so-called “Maintenance”), the body has a significant metabolic adaptation as a response to this weight loss such that with a loss of 10% of the body weight (20 pounds for a person who started at 200 pounds), the metabolism drops by 300-400 calories per day.
In addition, thyroid balance changes, so people feel like they are low in thyroid hormone (cold, thin hair, dry skin) even with thyroid hormone levels are measured as normal, and muscle efficiency improves, so that walking a mile now burns 20% less calories than before losing the weight (“Hypometabolism”).
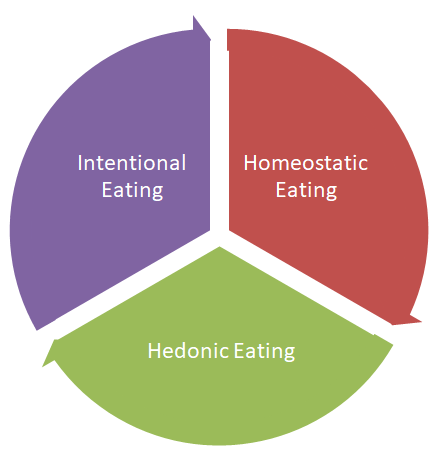
Further, for each kilogram lost (2.2 pounds), the appetite increases by 95 calories per day while the energy expenditure decreases by 25 calories per day. After weight loss, one gets hungrier before eating, feels less satisfied after eating, and gets hungrier again sooner than prior to the weight loss due to hormonal mechanisms. And the greater the weight loss, the greater the changes.
Studies like these demonstrate why we need to stop talking about “Maintaining” weight loss. Instead, we need to discuss “Optimal Treatment.” Maintaining sounds easy – just keep doing what you’re doing. Weight loss has stopped so the medication can be stopped. But it ignores these metabolic adaptations which make sustaining weight loss (a.k.a. “Maintenance”) exponentially more difficult than losing it was in the first place!
Instead, let’s focus on long-term treatment to improve health. I like to teach doctors and patients that obesity is a chronic but treatable disease. Treatment includes lifestyle intervention, healthy eating, physical activity, medical management, and sometimes surgery.
So how do you keep the weight off?
Focus on losing weight using strategies that are sustainable:
- Work on eating a healthy diet! Meal replacements are an evidence-based tool that can improve on the amount of weight lost.
- Be active every day! Time matters – try to find an hour a day.
- If medication(s) are used to help lose the weight, they should be continued for long-term treatment.
- Work on stress reduction and get enough sleep.
- Remember that we are here to support you – regular visits have been shown to help people achieve and keep off more weight.
- Don’t get frustrated because you didn’t lose as much weight as you’d hoped!
One of the most common questions I get is whether or not these metabolic adaptations get better over time. Dr. Rosenbaum showed data collected for 6 years showing that they persisted, again supporting the idea that we need to focus on long-term treatment. Hopefully by taking a long-term approach and not worrying about terms like weight loss and maintenance, we can instead focus on improving health, function, wellness and lifespan!



Dr Lazarus,
Thank you so much for your knowledge sharing and continued drive toward lifelong success with chronic disease management of obesity.
I am in the Optimal Treatment phase – and sent a note off Columbia to see if I may qualify for any of their research because I’m having a hard time finding translational medicine. It’s the ‘continue on long term treatment’ I’m looking for guidance on.
I agree, that chronic disease may require chronic medication management, but to use hypertension as an analogy, as BP meds are decreased and BP is monitored, there must be an arm of science that is considering how to optimize obesity where FDA-approved AOMs are concerned – or at least guidance related to dosing for both cost to the consumer and the provision of unnecessary treatment by practitioners.
Here’s me: 54 y.o. perimenopausal, hypothyroid, hypercholesterolemia – overweight last 40 yrs with obesity last 20. 5’4″ – highest weight 216 lbs – set weight at 195 lbs prior to starting oral AOMs. My weight loss with generic forms of Contrave & Qysemia plateaued at 177lbs over 1 year with a goal of 155 lbs, thus started Saxenda 3mg daily for the past 10 months to a weight of 150 lbs. I am currently reducing Saxenda in an attempt to wean myself for the past 6 weeks. Appetite resurfacing significantly, + sugar cravings, weight increased to 154 lbs in past 2 weeks.
I’m looking for the science or research surrounding the removal of the injectables. There must be some guidance out there other than to keep on the same medications that you lost the weight on. Either dose reduction or how to stop safety, should oral AOMs be stopped first or the injectables, are the GLP-1 inhibitors effective at a lower dose, and how to manage backorder?
I’m so grateful for a moment of your time in sharing your thoughts.
Thank you!
Thanks for the post – we generally continue the same treatment that was used to lose the weight in the first place. For this reason, it is important to choose safe effective treatment(s), whether oral, injectable, or both. It is “off-label” to use a combo (oral / injectable) but that is what we do with other similar diseases like type 2 diabetes. We continue at the treatment dose that was used to lose the weight – not a lower dose. Again, this is the same as diabetes – we don’t lower the dose of the glp-1 once we achieve a target a1c – we continue the treatment dose that was needed to get it there in the first place (ditto for blood pressure, cholesterol, depression, etc.)